Osteochondrosis generally refers to degenerative changes in any joint cartilage. Thus, this pathological condition can occur in all joints of the musculoskeletal system. However, the most pronounced symptoms, for example, headaches and headaches, as well as heart pain, are noted in the case of cervical osteochondrosis, that is, damage to the cartilage tissue betweenthe vertebrae of the cervico-brachial column.
According to WHO statistics, around 60% of Europeans suffer from osteochondrosis to one degree or another. In men, the disease manifests itself about 10 years earlier than in women. Representatives of the more severe sex face symptoms somewhere around 45 years old. The female half is aged 55 to 60, respectively. At the same time, experts are sounding the alarm bells about the ongoing rejuvenation of this disease. If you do not take timely measures, then literally over the next decade the number of 30-year-old patients with osteochondrosis will increase significantly.
Causes of osteochondrosis
Dystrophic changes in the pulp occur for a variety of reasons. The natural aging of cartilage tissue must be put in the first place, which, alas, is an objective and compelling circumstance. However, as mentioned above, this disease is getting younger, which is no longer associated with aging, but with other reasons.
In young patients, the disease occurs due to metabolic disorders associated, as a rule, with poor diet. The abundance of fats and the low vitamin content of foods is the reason why the cartilage literally begins to "starve" and goes into a state of dystrophy.
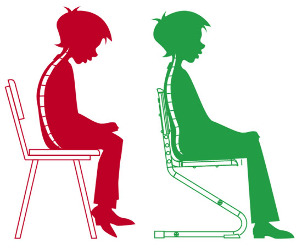
Another provoking factor is physical inactivity. Read the forums in which people who have encountered this disease communicate and you will see that most of them are still relatively young residents of mega-cities, which, as a rule, are engaged in mental work, involving a long sitting position. Low motor activity of the cervical vertebrae leads to loss of elasticity of the cartilage in the intervertebral discs.
Due to poor nutrition and associated metabolic disorders, as well as physical inactivity, the pulp begins to degenerate and becomes more and more dense. In the later stages of osteochondrosis, a complication occurs, which is manifested by the replacement of cartilage tissue with bone and thickening of the intervertebral discs. This leads to compression of the nerve roots and the blood vessels located here. The involvement of elements of the nervous and vascular systems in the pathological process determines the specific course of osteochondrosis.
Specificity of the disease
The difficulty in fighting this disease lies in its late diagnosis, which is explained by the disguise of osteochondrosis under other pathologies. People waste precious time and do not treat this pathology, because they are not aware of its presence. And patients cannot be blamed for it. If the pressure jumps, we treat the hypertension. Stabbed heart - we're going to cardiology. The head hurts regularly and now a person cannot fall asleep without ibuprofen or analgin. It doesn't even occur to us that we need to see a neurologist.
And during this time, a few visits to a specialist of this profile will allow you to start the process of restoring the cartilage of each cervical vertebra, which will gradually eliminate both false hypertension and suspicion of angina pectoris, constant headaches and other symptoms associated with the condition of the cervical region of the shoulderthe spine, it seems to us, does not seem related.Timely detection of pathology prevents further pulp dystrophy and allows you to treat osteochondrosis at home and on an outpatient basis - without hospitalization. Unfortunately, the lion's share of patients turn to a neuropathologist who already suffers from sufficiently severe damage to the intervertebral discs - when the neck begins to ache unbearably.

Diagnostic methods
Diagnosing osteochondrosis is a complex job. The research can take a long period of time, but its costs are justified, as early treatment of this disease avoids the worst-case scenario - surgery to replace the ossified intervertebral disc, during which pinched nerve roots are released and implantsfunctional or simple height compensators are installed. Element removed from the spine. The type of solution required for a particular patient is determined by the orthopedist after a complete diagnosis.
Since the disease, as shown above, is masked, one must first ensure that the symptoms are not associated with problems in other organs. For example, if there is pain in the heart, you should undergo a cardiological examination and confirm the absence of heart disease. A full diagnosis will not only confirm the suspicion of osteochondrosis, but also learn about the general condition of the body along the way.
The final diagnosis is made on the basis of the results of the radiographic examination of the cervicobrachial spine in frontal and lateral projections. A more informative method is magnetic resonance imaging (MRI). It allows you to more accurately determine the localization of dystrophic changes. Thanks to this, the doctor has the opportunity to prescribe one-off treatment.
Treatment with folk remedies at home
The advantage of osteochondrosis, if this word is used in this case, is that the patient can be treated at home, without compulsory hospitalization. The course of treatment includes taking special drugs and performing exercises of the exercise therapy complex.
Drugs (their types) used for the treatment of osteochondrosis at home are shown in the following table.
| Analgesics | In most cases these are tablets, sometimes capsules. These funds are designed to relieve pain in the cervical spine. |
| Anti-inflammatory | Hormonal drugs that stop the inflammatory process resulting from changes in the intervertebral cartilage. Also relieves pain. |
| Chondroprotectors | Medicines containing components for the restoration of cartilage tissue, such as hyaluronic acid. Designed for long term use. |
| Muscle relaxants | Means for relieving muscle tension. These drugs are taken only under the supervision of an attending physician. Limited use due to the large list of contraindications. |
| Exterior | Ointments, gels and so on. Anti-inflammatories, pain relievers and heaters are used. Before using these funds, you need to consult a specialist. |
| Vitamins | Preparations containing vitamins which improve the conductivity of nerve fibers and the functioning of the peripheral nervous system in general. These are group B vitamins, as well as vitamins A and C. In some cases, vitamin D is prescribed. |
It should be understood thatour list of types of drugs does not justify self-medication. A specific agent with an indication of the dosage and taking into account the pathogenesis in each individual case can be prescribed only by a registered neurologist. The thoughtless adherence to television advertisements "recommending" the best drugs against osteochondrosis does not come up against a cure for this disease, but on the contrary with a worsening of the situation. PAY ATTENTION!
Injection therapy
In the treatment of osteochondrosis, in addition to taking pills and applying ointments, the injection of drugs is used. There is a wide range of drugs for injection. Treatment courses include all types of injections, including the following:

- subcutaneous;
- intramuscular; intravenous
- ;
- epidurals.
injections are more effective than oral medications and all kinds of folk remedies. The blood flow quickly sends the agent to the sore spot, which explains the rapid healing effect. And, for example, with an epidural injection, the drugs are injected directly into the spinal cord and begin to work instantly.
Vitamins and other supportive drugs are usually injected subcutaneously. Anti-inflammatory drugs and chondroprotectors are injected intramuscularly. For example,injections of an anti-inflammatory drug, which are so popular with patients, are injected into muscle tissue. The drugs are injected intravenously to speed up circulation in the brain. This is necessary in the event of compression of the intervertebral discs invaded by blood vessels, through which the blood carries oxygen and nutrients to the brain. Epidural injections are given for the purpose of blocking severe pain when other pain relief methods are ineffective. With this injection, the needle passes between the vertebral processes and delivers the anesthetic directly to the spinal cord. This procedure is performed only by a qualified professional anesthesiologist.
Injections are only fully effective if you exercise regularly in medical gymnastics. That is, in itself, the administration of drugs is not sufficient for the complete treatment of osteochondrosis. Only in combination with exercise therapy is it possible to relieve the symptoms of the disease and, in the future, restore the affected cartilage tissue.
What to do during exacerbations?
Although osteochondrosis of the cervical spine is chronic and more or less imperceptible for long periods of time, patients sometimes face exacerbations. In each patient, they occur at different intervals and can occur unpredictably. During these times, it is important to take timely action in order to avoid a significant deterioration of the condition.
Provocateurs exacerbation
Exacerbations of osteochondrosis, as in any other disease, do not happen, as they say, out of the blue. Usually, acute conditions are caused by the following factors:
- stress;
- non-professional massage;
- meteorological phenomena;
- visit of a thermal bath (sauna);
- excessive physical activity after prolonged physical inactivity.
In women, osteochondrosis is often exacerbated during menstruation. Alcohol abuse is also a powerful provocative factor.
Symptoms of exacerbation
The symptomatology of exacerbations of osteochondrosis in each patient manifests itself differently and is determined by the general clinical picture of pathogenesis. For example, neck and headachesin acute conditions are noted by all patients, and loss of sensitivity to numbness of the face during exacerbations is not felt by everyone, but it does happen quite often. And, of course, during this period the symptoms of those diseases under which osteochondrosis is masked are exacerbated. These are heart pain, dizziness, tinnitus, hot flashes, etc. Especially dangerous are exacerbations, during which inflammation of the cervical spine occurs.
Relief measures for exacerbations
In times of aggravated osteochondrosis, you should first consult your doctor. There is no need to ignore this rule, as delay in this matter can do a disservice. The neurologist will assess the patient's condition and recommend measures for an effective and, above all, safe way out of the crisis.
Usually, in acute conditions with osteochondrosis, injections of analgesics and anti-inflammatory drugs are prescribed. But gymnastics during this period should be discontinued. On the contrary, the patient should remain calm. Kneading the neck is unacceptable - it can make the condition worse. It is advisable to transfer the aggravation to the supine position and fix the head at the same time, placing a roll or at least a rolled sheet underneath.
An important place in reducing the frequency of exacerbations is their prevention, which boils down to maintaining the right engine speed on a daily basis.A patient with osteochondrosis should watch their posture, keep their head straight, avoid sudden movements. In wet and cold weather, it is necessary to protect the cervical vertebrae from hypothermia. And, of course, you should not forget about medical gymnastics for a minute - you should do it regularly. This is the key to the development of osteochondrosis without exacerbations.
2 degrees of illness
Neuropathologists distinguish 3 degrees of osteochondrosis - 1st, 2nd and 3rd respectively. In the lion's share of patients, the disease is recorded in the second stage. This is due to the following points. The disease of 1 degree is characterized by the appearance of short-term pain in the neck, resembling an electric shock. At the initial stage, the fibrous ring, which holds the central part of the intervertebral disc, begins to collapse. The guideline for the diagnosis of grade 1 osteochondrosis is dilation of the pupils, which is not associated with other phenomena in the body.
The number of patients with grade 1 osteochondrosis is not very high. The disease at this stage is transient and is either eliminated (with timely treatment), or quickly passes into the second stage - if the moment is missed. The situation for the number of patients with grade 3 osteochondrosis is similar. He is also small. This is due to the fact that most often doctors manage to start treatment in a timely manner and prevent the pathology from passing from the second stage to the third. The disease of this degree is characterized by symptoms such as sharp neck pain, which does not go away even after taking painkillers, partial loss of control of the upper extremities, constant dizziness and often fainting. Third-degree osteochondrosis is treated, as a rule, with surgery, since drug therapy is often ineffective.
Since most patients suffer from 2nd degree osteochondrosis, this form of the disease is of the greatest clinical interest, and it is in the treatment of the disease at this stage thatthe greatest experience has been accumulated. According to statistics, the proportion of patients with stage II osteochondrosis among all patients with this pathology is about 75%.
The specificity of this form of the disease is its chronic course with short periods of exacerbation.The second degree differs from the first in the continuous decrease in the space between the vertebrae. That is, the intervertebral disc has not yet collapsed, as in the case of the third stage, but it becomes considerably thinner, which leads to pinching of the nerve roots and causes all the classic symptoms of osteochondrosis.
The pathology of the 2nd degree being the most widespread, speaking of the treatment of cervical osteochondrosis in general, they involve the implementation of therapeutic measures in relation to this particular form of the disease. And they include, we repeat, drug therapy and physiotherapy exercises. Properly carried out treatment allows you to eliminate the disease and prevent its transition to the third stage with an almost inevitable operation to replace the intervertebral discs.
Main symptoms and appropriate treatment
Osteochondrosis of the cervical spine is a difficult to diagnose degenerative lesion of the intervertebral discs. Most often it is encountered by people aged 45-50, but in recent years the pathology has "rejuvenated", and now neuropathologists often admit patients aged 30 years.
The difficulty in detecting osteochondrosis is due to the "simulating" nature of the course of the disease - when it is disguised as other pathologies.The cause of the disease is the deterioration of the elasticity of the cartilage tissue, which forms a cushioning pulp between the vertebrae. The cartilage becomes thinner and denser. As a result, the nerve roots are compressed (this is called root violation), resulting in the following symptoms:
- pain in the head and heart;
- increased blood pressure;
- decreased sensitivity in the facial area (to numbness);
- partial paresis of the upper limbs.
All of these symptoms are certainly accompanied by neck pain. Often this pain is mild and does not require the patient to take pain relievers. Ignoring the slight pain in the neck, the patient does not raise the alarm on osteochondrosis, but tries to treat other pathologies, for example, angina or hypertension, which he probably does not have.
Processing methods
According to modern approaches, osteochondrosis occurs in waves. At first, it manifests itself in the form of an exacerbation (acute period). Then the symptomatology weakens and a subacute period sets in. The third stage is remission, the condition of which continues until the next exacerbation. The task of the treatment of osteochondrosis is to quickly stop the acute phase, relieve the patient's condition in the subacute period and ensure long-term remission.
During the acute and subacute phases, the patient takes pain relievers and anti-inflammatory drugs. At these stages, an effective solution is the use of a Shants gauze collar, which gives the head a position in which the neck muscles relax, which eliminates the pain. During the period of remission, drug therapy with chondroprotectors that improve the quality of cartilage tissue and a set of exercise therapy physical exercises are indicated. Exercise is even more important than hyaluronic acid injections because healthy physical activity naturally stimulates the formation of collagen fibers in cartilage.
Type of cervicothoracic pathology
Strictly speaking, cervical and thoracic osteochondrosis are two different forms of the disease. However, they are often combined. This is due to the fact that the cervical and thoracic spines are closed with each other, which connects these two types of pathology of intervertebral discs. That is, with dystrophic changes in the cervical vertebrae, practically the same violations are observed in the thoracic region. Therefore, these two forms of the disease are combined, especially since their symptoms are very similar. The main symptom is pain. With cervical osteechondrosis, the pain is localized in the neck, in the case of cervicothoracic lesion, pain in the sternum is added to it.
Common symptoms are:
- numbness of the face;
- head and heartache;
- instability in blood pressure;
- loud tinnitus.
In case of damage to the thoracic vertebrae, the list is supplemented by impaired coordination of movements, activation of osteoarthritis of the shoulder joints, numbness of the hands.
Treatment of the cervico-thoracic spine
Treatment is prescribed after a thorough diagnosis using X-rays or magnetic resonance imaging (MRI). Treatment of osteochondrosis is complex - drugs and physiotherapy. Pharmacotherapy involves the use of anti-inflammatory and analgesic drugs.An important part of the treatment is the use of chondroprotectors which directly restore the cartilage tissue in the intervertebral space. Physiotherapy measures include compresses and the use of all kinds of ointments, as well as physiotherapy exercises.
If osteochondrosis is detected in the thoracic spine, professional massage is indicated. The massage effects trigger the natural processes of regeneration of cartilage tissue. Massage is more effective in eliminating the disease of the thoracic vertebrae than gymnastics, since the spine in this place is not flexible, and therefore, when performing exercises, it is not always possible to providenormal range of motion for individual vertebrae. A massage therapist, on the contrary, is able to have a precise effect on a diseased intervertebral disc. Only you need to contact a specialist in spine massage who has an appropriate certificate. Additionally, the massage therapist must be licensed.
Timely measures to rule out cervicothoracic osteochondrosis will prevent surgery to replace an intervertebral disc destroyed by a stent. Early diagnosis of pathology and discipline in outpatient treatment with drugs and folk remedies will save you money. If you have the slightest suspicion of osteochondrosis, see a neurologist. But better. . .
Be sure to consult your doctor before treating any illnesses. This will help take into account individual tolerance, confirm the diagnosis, ensure that the treatment is correct, and rule out negative drug interactions. If you use prescriptions without seeing a doctor, it is at your own risk. All information is presented for informational purposes only and does not constitute medical aid. All responsibility for the application lies with you.



































