
General information
A disease of the human musculoskeletal system such as osteochondrosis is essentially a degeneration of the articular cartilage and surrounding bone tissue, with frequent involvement of adjacent vessels, muscles and nerve endings in the pathological process. In principle, this term can mean a number of osteoarticular pathologies of various localization, including with the joints of the extremities, but most often it is used to denote degenerative-dystrophic changes in the structure, directly the spine and, above all, the intervertebral discs.
Due to the progression of intervertebral osteochondrosis, the human body loses its inherent shock absorption qualities, mobility and elasticity. In general, this disease of the spine is very common and to a different degree or degree of severity is present in most people by the age of 40. Depending on the segment of the spine affected in clinical practice, cervical, lumbar and thoracic osteochondrosis, as well as their mixed forms, are considered to be the most difficult.
Osteochondrosis of the thoracic spine, which will be discussed in this article, is the rarest form of this pathology, which, in particular, is due to the anatomical structure of the upper part of the human skeleton. Then, at the level of the chest, the bone-cartilaginous system consists of 12 vertebrae, which are connected by means of joints with ribs, which, with their front ends, adjoin a relatively monolithic sternum. Such a skeletal structure sufficiently provides a rigid and strong framework that protects the organs of the thoracic cavity (heart, lungs) from injury. In addition, the vertebrae in this segment of the spine are characterized by a low height and significant length of the spinous processes, which gives them closely spaced tiles. All of this together limits the mobility of this part of the back and the negative impact of physical activity on it, protecting the intervertebral discs from destruction.
As another reason for the lower frequency of detection of osteochondrosis of the chest in a person, compared to lumbar and cervical osteochondrosis, physiological kyphosis (natural bending of the spine backwards) ispresent in this area, due to which most of the external load falls on the anterior and lateral fragments of the vertebrae and discs. With the development of a pathological process in the motion segment of the spine, it is these areas that are primarily prone to degenerative changes, however, due to the lack of nerve endings and membranes of the spinal cord, painis most often not observed. Nevertheless, in some cases, negative transformations in the thoracic segment of the spine affect posterior fragments of discs and vertebrae and / or vertebral-costal joints, which often leads to compression of the roots of the spinal nerves. Under such conditions, osteochondrosis of the thoracic spine occurs with radicular syndrome, which is alreadyaccompanied by pains of various localization (sometimes very distant), as well as a violation of the functionality of many organs of the human body (liver, lungs, pancreas, heart, etc. ).
Due to these ambiguous and varied manifestations of thoracic osteochondrosis, doctors often call this form of pathology "chameleon disease", because it can skillfully disguise itself as symptoms of respiratory and digestive diseases, heart muscle, etc. In this situation, a correctly conducted differential diagnosis is very important, which, thanks to various specific studies, will help to determine the symptoms and treatment of osteochondrosis of the thoracic spine.
The tactics and effectiveness of further treatment will largely depend on the degree of progression of the degenerative-dystrophic process in the tissues of the spine. Having recognized the pathology in the early stages of its development, it is important to improve the patient's conditionit is quite possible with the help of simple physiotherapeutic techniques and exercise therapy exercises, but in the casefrom its late detection, it may be necessary to perform a complex surgical operation. This is why doctors-vertebrologists strongly recommend any frequent and / or prolonged back pain as soon as possible seek the help of a specialist.
Pathogenesis
The incidence of osteochondrosis of the thoracic spine in women and men is practically the same, since in the pathogenesis of this disease there is no gender predisposition to the appearance of degeneration of theintervertebral disc. Nevertheless, many years of clinical experience in the treatment of osteochondrosis indicate that its first symptoms in men appear at an earlier age than similar negative symptoms in women. In particular, this is due to the fact that the osteochondrals tissues of the female body until a certain age are protected by the hormone estrogen, a decrease in the level of which at the time of climacteric transformations serves as a trigger for spinal problems.
According to statistical evidence, in general, intervertebral osteochondrosis of varying degrees of severity is observed in most older people, which automatically classifies it in the group of age-related diseases. During this time, the last time is followed by a significant "rejuvenation" of this pathology, until its appearance in preschool age. For this reason, it has not been possible to establish the exact etiology and initial pathogenesis of spinal osteochondrosis until today. At one time, more than a dozen theories about its origin and development were developed, including hormonal, infectious, mechanical, vascular, hereditary, allergic, and others, but in practice none of them found confirmation. complete.
Today, doctors explain the occurrence of osteochondrosis by the sum of the complementary negative effects on the tissues of the spine, among which a constant excessive load on one or more movements of the spinesegments formed by two vertebraeadjacent (upper and lower) and a disc located in the middle of them. Paradoxically, such an overload can be the consequence of both excessive physical work on the spine and the long-term result of finding an unnatural position for the back. For example, prolonged work or studies while sitting at a table is one of the main factors in the development of degenerative-dystrophic changes in the structure of the intervertebral. disk.
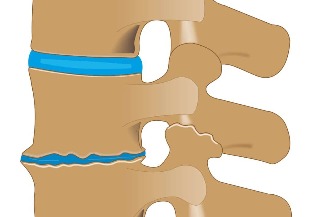
The initial formation or exacerbation of osteochondrosis of the thoracic spine can be influenced by improper nutrition, uneven development of back and pectoral muscles, excessive weight (obesity), pathology of the lower extremities (for example, flat feet), back injuries, etc. In the pathogenesis of this disease, the disorganization of segmental blood circulation plays an important role, which causes dehydration of the nucleus pulposus (gelatinous), which in turn leads to loss of damping qualities of the intervertebral disc, change in loads onsurrounding fibrous ring and further progressive destruction of this segment of spinal movement.
During its progression, thoracic osteochondrosis goes through 4 consecutive stages of development, each characterized by its own anatomical and morphological changes in the structure of the disc, adjacent vertebrae, and facet joints. In addition, negative metamorphoses that occur with this disease can directly affect other nearby tissues (muscles, vascular, connective) or indirectly affect the work of distant organs and systems of the human body. (intestines, heart, lungs, etc. ).
First degree
At the initial stage of the formation of thoracic osteochondrosis, microcracks are formed in the inner membrane of the annulus fibrosus, into which the nucleus pulposus gradually begins to penetrate, irritating the nerve endings in the distal layers of the fibrous rings andin the posterior longitudinal ligament. At this stage in the development of the disease, the patient may already feel pain directly in the middle part of the back or noticeable pain in the region of the heart. He may also be haunted by a feeling of convulsive contraction. in the back muscles.
Second degree
Osteochondrosis of the thoracic spine of the 2nd degree is characterized by further destruction of the fibrosus ring, which is accompanied by instability of the spine, resulting in excessive mobility of its affected vertebrae. Painful sensations of the 2nd degree of development of the pathology intensify and can proceed in the form of back pain (persistent mild pain, aggravated by back movements) or back pain (occurring suddenly against the background of a prolonged stay in one positionshooting").
Third degree
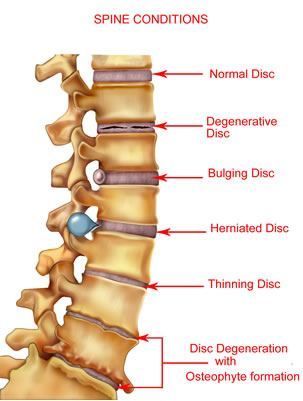
In the third period of thoracic osteochondrosis, there is a complete rupture of the structure of the fibrous ring with the exit of the nucleus pulposus beyond its borders and the formation of an intervertebral hernia. Most often, such formations occur in the direction of the canal vertebrae, which leads to compression of the spinal cord, spinal nerves and adjacent vessels. This is accompanied by radicular syndrome (pain radiating to different parts of the body), chest pain on the background of osteochondrosis (severe pain behind the breastbone, resembling heart), myelopathy (sensory and movement disturbances) and other symptoms. neurovascular and musculo-tonic in nature. Fixed thoracic kyphosis, scoliosis, or kyphoscoliosis may begin at this stage.
Fourth degree
During the final stage of thoracic osteochondrosis, degenerative processes spread to interspinous and yellow ligaments, other tissues of the spine and neighboring muscles. Intervertebral disc dystrophy continues to progress, until sacicatrisation and additional fibrosis. Deforming osteoarthritis develops in the lunar and intervertebral joints, osteophytes (bone growths) are formed on the processes of the vertebrae. The clinical picture at this period of the disease can be quite versatile, since the degree of damage to individual discs is often different. In uncomplicated osteochondrosis, problematic disc fibrosis can mark the progression of the disease to the stage of stable remission, but with loss of normal functionality to one degree or another. spine.
Reasons
Thoracic osteochondrosis in men and women can develop due to the following predisposing factors:
- the natural process of physiological aging, accompanied by age-related changes in the structure of the bone-cartilage tissue of the spine;
- genetic predisposition to the abnormal formation of motion segments of the spine;
- a physically inactive lifestyle leading to dystrophy of the back muscles;
- strength sports that involve excessive mechanical stress on the spine (mainly weight lifting);
- injuries to the spine (even those which occurred in the distant past);
- endocrine disorders in the human body, disrupting the nutrition of the tissues of the spine;
- significantly above normal body weight (obesity);
- unhealthy diet (lack of vitamins, minerals and fluids);
- pathology of the spine with its unnatural flexion;
- imbalance in the development of muscle structure;
- prolonged study or working in a sitting position with the body tilted forward;
- physically difficult working conditions (incorrect constant weight lifting);
- severe metabolic disorders;
- flat feet and other diseases of the lower extremities, affecting the redistribution of loads on the spine;
- vascular diseases that affect the blood supply to the back;
- severe infectious, allergic and autoimmune processes;
- frequent hypothermia;
- stressful situations and nervous exhaustion;
- bad habits and smoking.
Symptoms of osteochondrosis of the thoracic spine
Signs of thoracic osteochondrosis, due to the above-described structural features of this segment of the spine, may not directly bother the patient for a long time and only appear if the pathological process spreads to theside and / or posterior parts of the affected spinal movement segments and the transition of the disease to the second or third degree. In general, all symptoms of thoracic osteochondrosis are expressed as vertebral syndromes (painful effects directly related with functional disorders in the bone-cartilage tissue of the spine) and extravertebral or compression syndromes (negative phenomena resulting frompathological impulses of the problematic segment of the spine).
Vertebral syndromes
The vertebral symptoms of osteochondrosis of the thoracic segment of the spine are mainly manifested by two pain syndromes, called back pain and back pain.
Dorsago
This is a sudden, sharp attack of pain called “lumbago, ” localized in the interscapular space and can occur at any time. Most often, dorsago syndrome affects patients who have been in a sitting position with the body tilted forward and suddenly changing the position of the body. Patients describe the very moment of the attack as a "stab" accompanied by a sharp spasm of the spinal muscles. In addition to severe pain, subjective sensations with the dorsalexpressed by shortness of breath and a significant restriction of freedom of movement in the thoracic part of the back. A similar exacerbation of osteochondrosis with periodic attacks can last up to two weeks.
Back pain
This syndrome differs from the previous one by the gradual development of uncomfortable and painful sensations, which may increase over the course of two to three weeks. The pain itself with back pain is not so pronounced, but its prolonged presence causes a constant feeling of anxiety. The back muscles, as well as during the back muscle, are under great stress, which can cause the patient to feel a lack of inhaled air. Back pain increases with trunk movements (especially when bending down), deep breathing, coughing, etc. Upper back pain (main location of negative phenomena in the cervicothoracic segment of the spine) and lower back pain (main location of negative phenomena in the thoraco-lumbar segment of the spine).
Extravertebral syndromes
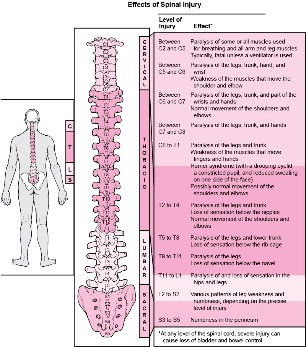
The extravertebral syndromes of thoracic osteochondrosis, due to the greater extent of this part of the spine, can be very diverse, which greatly complicates the correct diagnosis of the disease. They arise as a result of the compression of the corresponding nerve roots, neighboring vessels or the spinal cord itself. Symptoms of compression in men and women are usually similar and differ only when the pathological impulses spread to the sexesphere (for example, in men, against the background of the disease, sometimes erectile dysfunction is noted). In almost all cases, extravertebral symptoms are caused by already formed intervertebral hernias, which most often appear in the lower thoracic regions, but in principle they can form in any segment of the spine's movement. vertebra D1 to vertebra D12. As you can see in the image below, it is on the localization of osteochondrosis in them that involvement in pathologiesthe process of certain systems and organs of the human body with their characteristic negative manifestations.
Root syndromes
As part of the compression symptoms of thoracic osteochondrosis, radicular syndromes are most commonly and clearly seen, caused by compression of nerve endings in one or another segment of the spine. Depending on the concentration, such problems of patients can be disturbed by the following painful phenomena:
- for infringement in the area of the T1 vertebra - painful sensations and paresthesias of the movement segment of the upper thoracic spine most often spreading along the suprascapular zone in the area of theone of the armpits up to the elbow joint;
- for violation in the region of the T2-T6 vertebrae - pain such as intercostal neuralgia may extend from this part of the spine along the interscapular region and encircle the axillary and scapular areas in halfcircle, as well as 2-6 intercostal space in the sternum;
- in case of violation in the area of the T7-T8 vertebrae - the pain in the girdle mainly spreads from the lower level of the shoulder blades of the costal spinal joints to the upper parts of the costal arch and affects the epigastric region, where itcauses muscle defense (strong muscle tension);
- in case of infringement in the region of the T9-T10 vertebrae - intercostal neuralgia extends from the lower movement segments of the thoracic spine to the lower parts of the costal arch and further to the umbilical region, changing the tone of the mid section of the abdominal muscles;
- in case of violation in the area of the T11-T12 vertebrae - the pain also emanates from the lower segments of the movement of the thoracic spine and reaches the hypogastric (under the stomach) and groin areas along thecorresponding side areas of the chest.
In addition to pain, radicular syndromes of thoracic osteochondrosis are often accompanied by negative symptoms of certain internal organs of the abdominal cavity and / or chest. Moreover, in some cases, such symptomsare so similar to the pathological manifestations of other diseases that it is practically impossible to accurately recognize their belonging without directed research. For example, the medical literature describes a case of wrongful appendectomy (surgery to remove the appendix) according to the unambiguous clinic of acute appendicitis, which in fact turned out to be one of the pronounced syndromes of osteochondrosis. .
So, when the osteochondrotic process is localized in the upper thoracic region of the spine (from T1 to T4), patients may experience pain and / or various discomfort in the esophagus or pharynx, which is often seenlike the presence of a foreign body. Such sensations are often paroxysmal (sometimes permanent) and intensify with a large load on the problematic part of the back. Sometimes the manifestations of radicular syndrome in the upper thoracic segment are confused with signs obstructive bronchitis or pneumonia, since a reflex cough with osteochondrosis of the thoracic region and chest pain resemble the symptoms of this group of diseases. In addition, chest pain may occur in the form of chest pain, recalling its intensity is an attack of angina pectoris, pulmonary thromboembolism, myocardial infarction, and other similar pathologies of a serious nature, which require a detailed differential analysis of thefrom doctors.
Patients with osteochondrosis in the middle thoracic segment of the spine (T5 to T7) most commonly experience discomfort and pain in the solar plexus and stomach, called spinal gastralgia. On the defeatsegments of movement of the T8-T9 spine, it is possible to develop pain in the duodenal region, called - vertebrogenic duodenalgia. . . These two and other painful sensations in different patients or at different times can vary in intensity from mild and "painful" to extremely acute. They intensify, as a rule, with a prolonged stay of the body in one position (sitting at a table, lying on the back, etc. ), with sudden movements of the body, and also at the time of sneezing or sneezing. cough. Often these pains are accompanied by paresthesias. (numbness, tingling, burning) in the middle of the abdominal wall.
With radicular manifestations of osteochondrosis in the lower thoracic region of the spine (from T8 to T12), some patients may complain of pain in the lower abdominal cavity, mimicking intestinal disorders or pathology. sometimes the pain spreads to the gallbladder and is localized in the posterior region of the right hypochondrium. Even less often, patients experience pain similar to the pathological bladder clinic in the suprapubic region. As in the previous case, the nature of such pain can vary over a fairly wide range (from mild to severe), and its severity increases with prolonged physical or static stress on the spine, sneezing, coughing, etc. .
Compression myelopathy
This compression syndrome of thoracic osteochondrosis is quite rare and is a compression of the spinal cord directly by the resulting intervertebral hernia. . . Its characteristic symptoms at the beginning of the formation is expressed by local pain in the corresponding area of the back or pain in the belt in the problem area, as well as a feeling of weakness and / or numbness in the legs. With progression, the pain intensifies, it can affect the lower intercostal space, abdominal organs, groin area and significantly felt in the lower extremities. In severe cases against the background of compression myelopathy, a dysfunction of the pelvic organs may develop, leading to disruption of the processes of defecation and / or urination. In addition, there may be severe superficial and deep paresthesias and sensory disturbances, up to spastic paresis in one or even both legs.
Vascular compression
Compression of the vessels adjacent to the thoracic segment of the spine leads to myeloischemia, as a result of which the blood supply is disturbed, and therefore the adequate nutrition of the spinal cord. Manifestations of this syndrome are, in fact, completely repeat the symptoms of compression myelopathy, and are mainly characterized by pelvic disorders, as well as loss of sensation in the lower extremities and decrease in their functionality. Patients often describe this problem with the phrase - "legs fail".
Vegetative syndromes
In a number of cases, with thoracic osteochondrosis, the vegetative nerve ganglia (ganglia) are damaged, which can lead to a wide variety of negative symptoms in the patient. These can be various paresthesias. , itching and changes in the pigmentation of the skin in the problem node area, burning pain in half of the body, local temperature disturbances, muscle hypertrophy or wasting, disorganization of the work of limbs or internal organs, etc. According to his, in fact, these visceral vertebrogenic symptoms are similar to the manifestations of radicular syndromes, but differ from them in the absence of clear localization and the presence of secretory and motor disorders. When involved in the pathological process of a star, a node affecting the upper thoracic vertebrae, there may be abnormalities in the arms, chest and heart. In case of damage to the lower thoracic nodes, functional disturbances may occur organs of the small pelvis, abdominal and thoracic cavity, as well as trophic changes in the lower extremities and the rest of the body.



































